The Early Years (0-5)
Chapter 4 – Health connections

CP is a lifelong condition, and the impact of some of the physical conditions can change as your child grows. Health services will help to watch or monitor any changes as your child develops.
Key points:
- Your child’s CP will affect different parts of their body and can change as they grow and develop.
- Building connections with health and education services is important as everyone will need to be involved to monitor changes over time.
- Connections with health and education services will be different for everyone and depends on factors such as your whānau and child’s needs and priorities, and where you live.
- The first connections are with your GP and Well Child Tamariki Ora provider.

“Your focus will shift, so just concentrate on what is
important to you right now.”
– Family quote


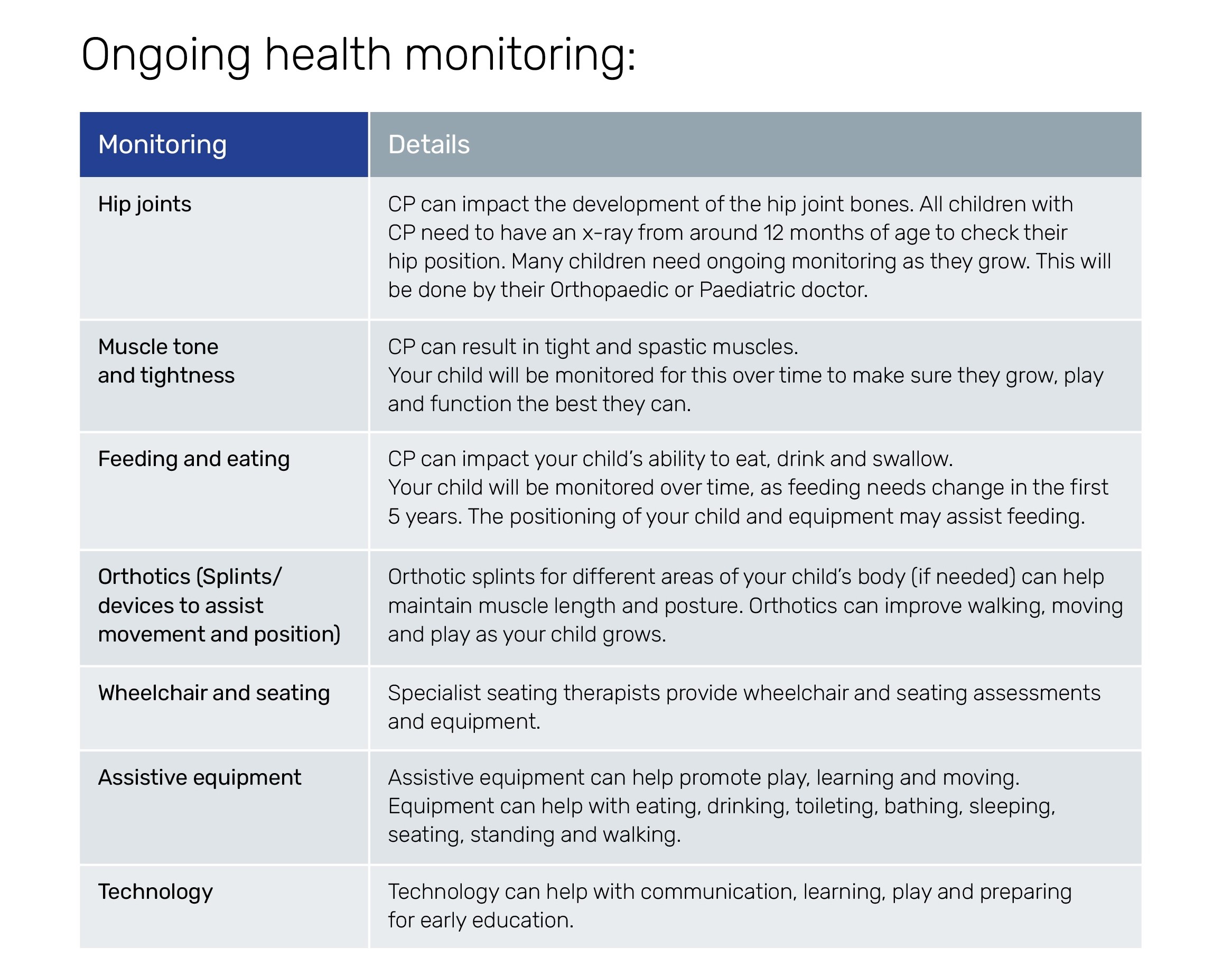
Monitoring specific health needs in CP
Monitoring hip joints with CP
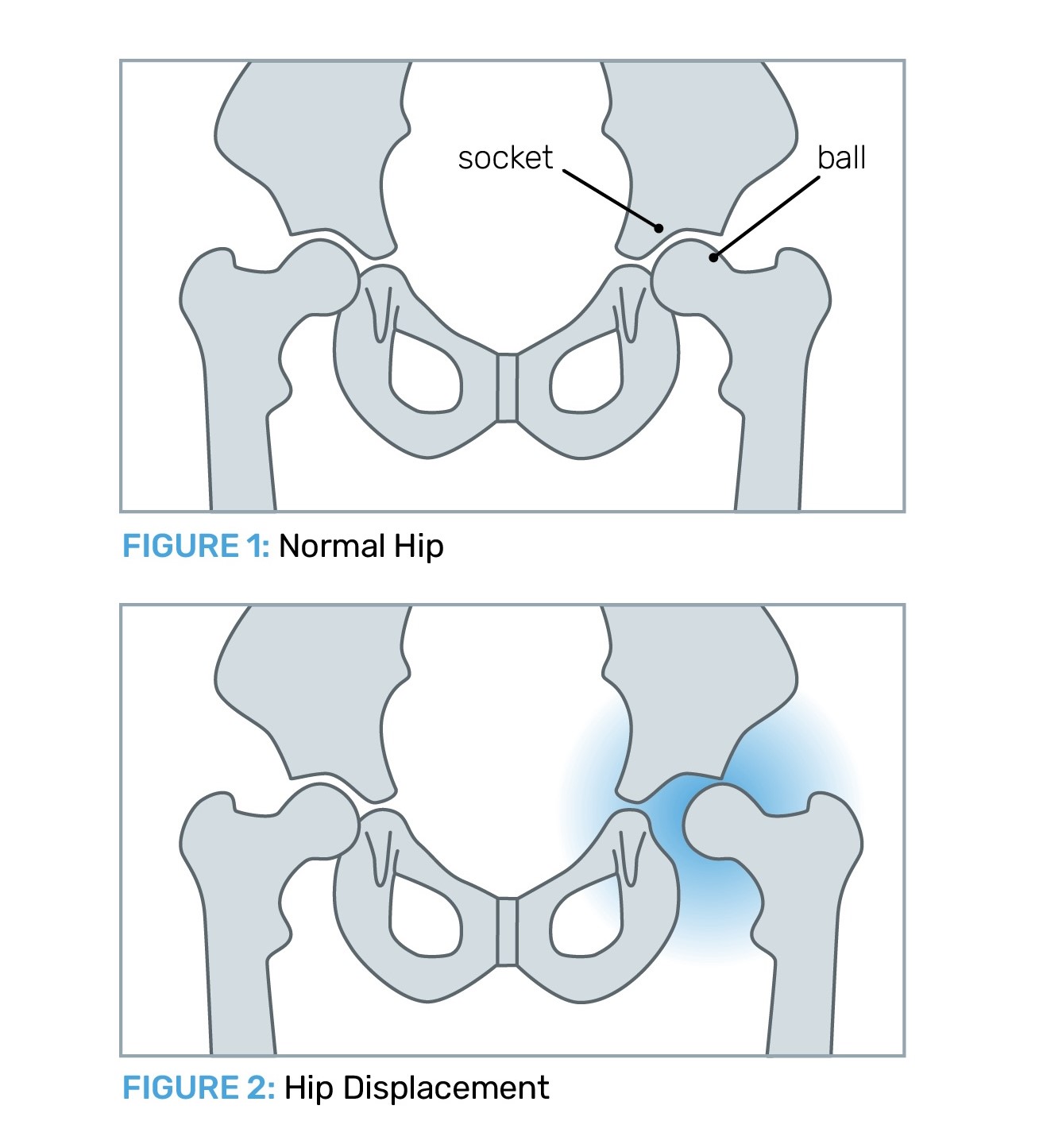 Children with CP can have problems with the position of the hips as they grow. This can be called different terms including hip displacement; hip dysplasia; hip subluxation or hip dislocation.
Children with CP can have problems with the position of the hips as they grow. This can be called different terms including hip displacement; hip dysplasia; hip subluxation or hip dislocation.
Children with CP who have limited walking ability have a higher chance of hip problems.
Hip problems may be due to a combination of tight muscles (spasticity) in the hip muscles and/or changes in the development of the shape of the bones as your child grows.
Finding out about hip problems early can help prevent the problem getting worse.
What is hip surveillance or monitoring?
- Surveillance means watching and checking.
- Hip surveillance includes a combination of regular hip (pelvis) x-rays and checking for clinical signs and symptoms, such as hip pain or restricted movement in the legs.
- Hip surveillance frequency is different for each child – it may be every six or 12 months.
- Changes in hip position can happen fast as children grow so quickly.
Who organises hip surveillance?
Orthopaedic services; rehabilitation paediatrician specialists; paediatricians and physiotherapists.
What are the treatments for hip displacement?
- Surveillance or monitoring of hip development over time.
- Treatment for tight muscles – botulinum toxin (Botox®) injections and/or surgery to lengthen tight muscles.
- Treatment for bony abnormalities – surgery to correct the position of the hip and pelvic bones.
- See: https://starship.org.nz/guidelines/hip-surveillance-in-cerebral-palsy/
Spine surveillance:
Older children (approximately 8 years and older) who use wheeled mobility aids such as wheelchairs need to have the curve of their spine monitored.
An Orthopaedic Surgeon or Physiotherapist will monitor the child’s posture, spine curve and the need for spine x-rays.
Monitoring eating, drinking and swallowing:
Some children with CP have challenges with swallowing different food and liquid textures, because of muscle weakness or coordination difficulties.
A Speech Language Therapist and other members of the Child Development team can work with you to make sure your child is eating and drinking effectively. They can help check swallowing, coughing, mealtime habits and for the presence of reflux (heartburn).
Therapists can advise on your child’s position when eating and drinking so that their trunk and head are properly supported. Changes to the consistency of food can also help your child swallow safely.
Some children who have ongoing feeding challenges may have an x-ray of their swallowing, called a videofluroscopy, to give more information so that the child is supported in the best way.
Other things that may be related to feeding difficulties:
- Frequent coughing or choking on saliva or during mealtimes.
- Drooling, excessive saliva.
- Presence of reflux (gastro-oesophageal reflux GORD – this is when stomach acid flows into the oesophagus – food pipe) – also called heartburn.
- Always sounding chesty or full of phlegm.
Respiratory health
Respiratory health is about having healthy lungs for breathing and doing everyday activities.
For some children the health team will be checking eating, drinking and swallowing as they grow, to make sure food and fluid does not go into the lungs over time (this is called aspiration), as aspiration may lead to chest infections.
If needed, a physiotherapist can help manage chest secretions to help keep the airways clear.
Who can I ask about feeding?
Talk with your GP, paediatrician or any of the Child Development team.
For more information on eating and drinking and lung health check out:
- New booklets explaining lung health to children with CP, developed in Perth, Australia
- A video on eating, drinking and CP, developed in the UK
- Details on the Eating and Drinking Classification System (EDACS) on the Starship website
- Eating and drinking information across the life stages on MyCPGuide Australia.
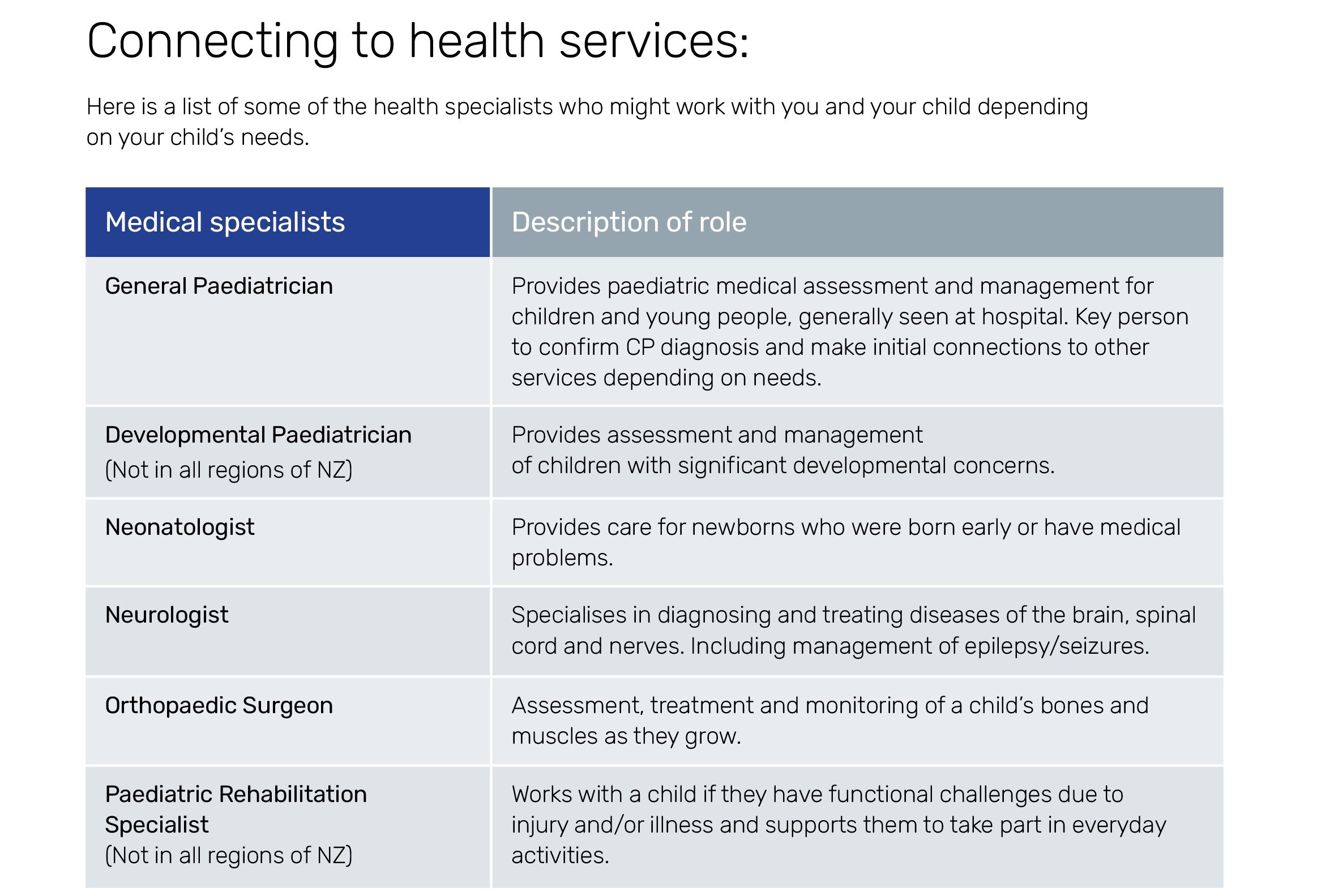
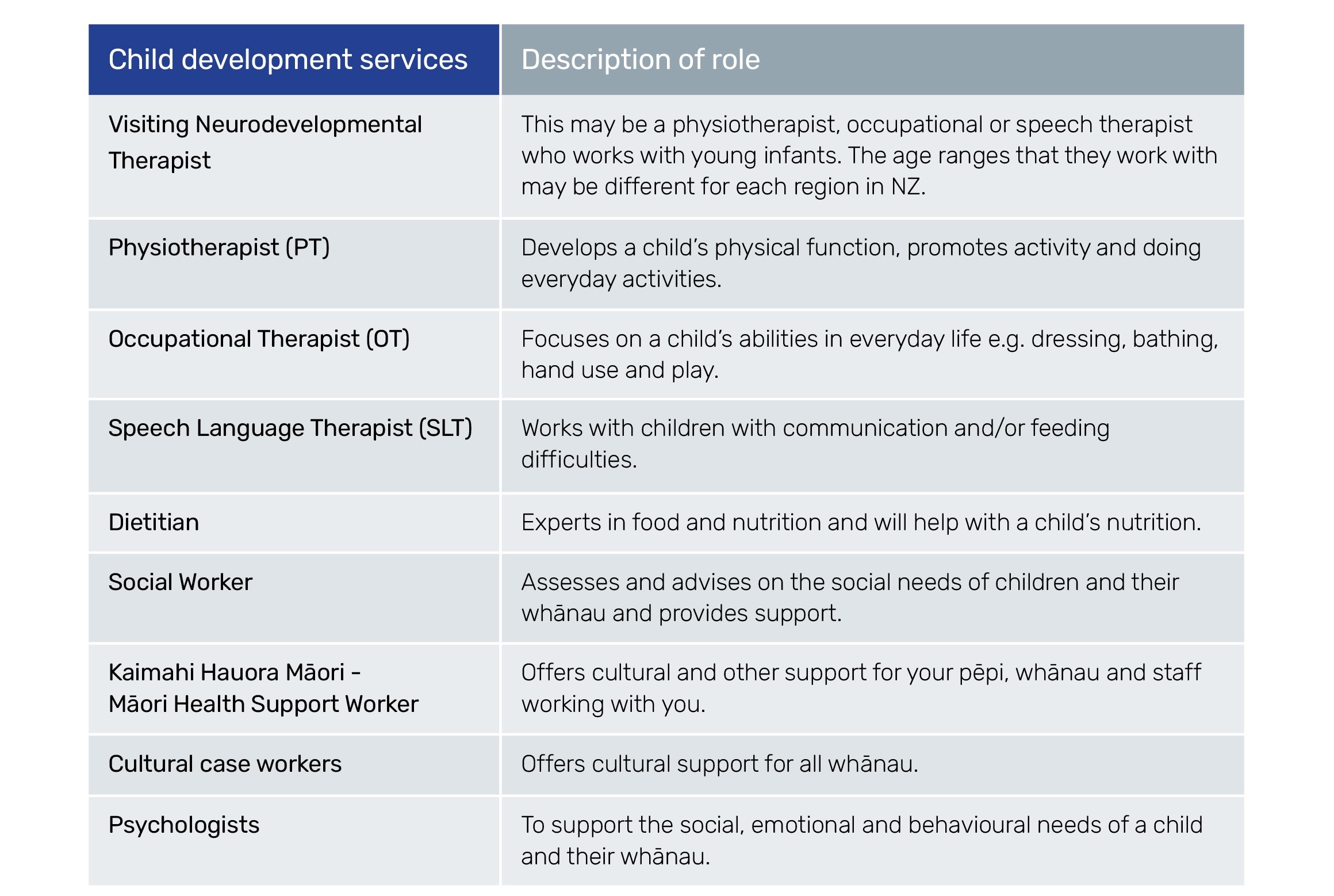
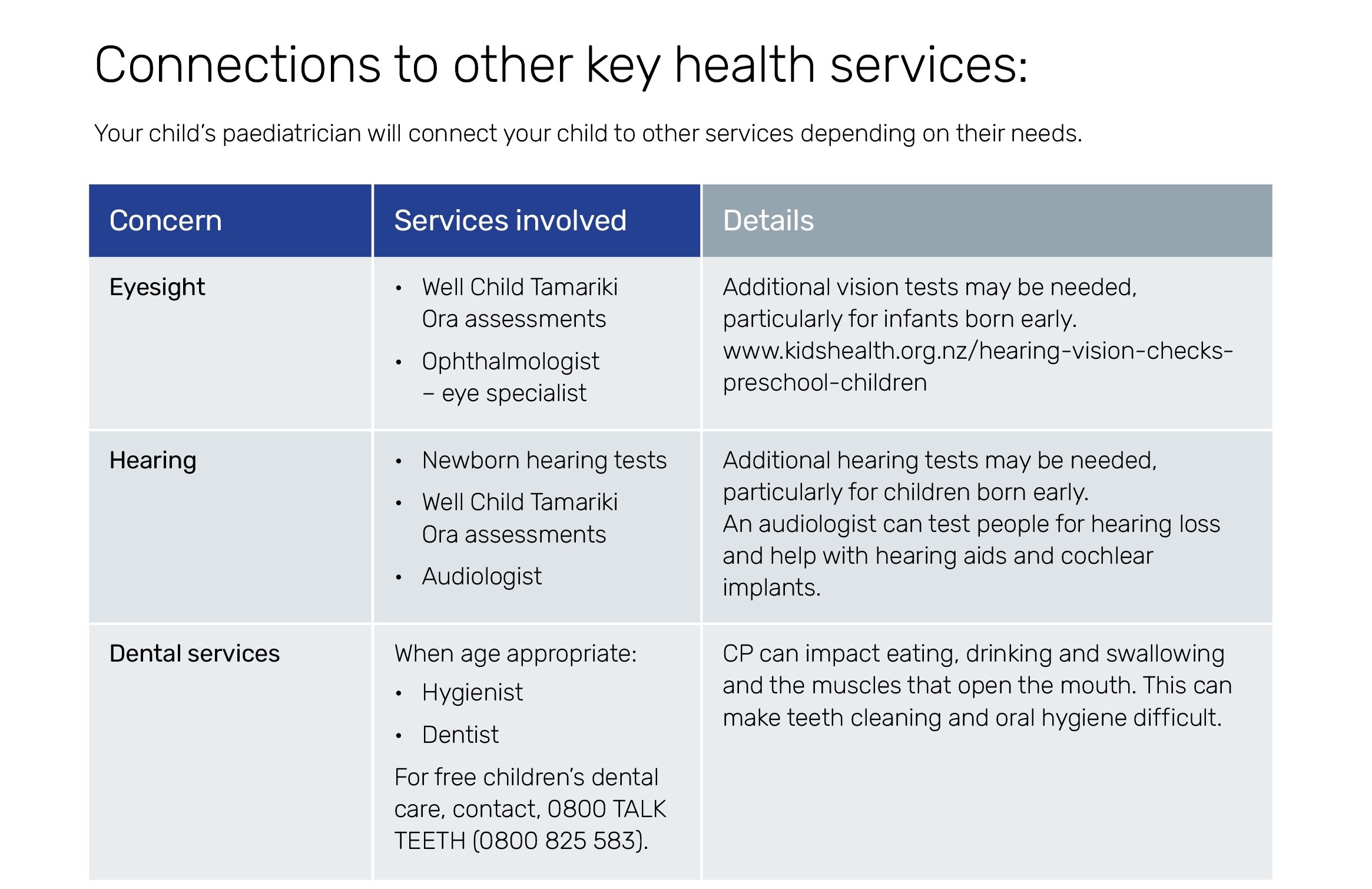
Who is in your child’s health team?
You can download this handy table to keep track of the people in your child’s health team:
Ideas for whānau
Sharing information
The physical impacts of CP are different for everyone. Some whānau find it helpful to make a list or chart the areas of the body that CP affects for their child, to share with people, such as carers or teachers. An example of information to share with day care teachers includes:
|
My child Noah has cerebral palsy (CP) which affects how he moves. Noah is great at:
Noah needs extra time for:
Noah will need your help:
|
You can include other areas that may be important or impacted due to CP:
- Breathing
- Dental
- Swallowing
- Nutrition and growth
- Saliva/drooling
- Constipation
- (Gastroesophageal) Reflux
- Hearing
- Vision
- Muscle tone and bones
- Pain
- Seizures
- Sleeping
- Speech and communication
Questions you can ask the health care staff working with your child and your whānau:
- If our child gets really unwell after hours, do we take them to ED or to the local after-hours service?
- Do I need to tell them about all our child’s health, or will they be able to access hospital records?
- Is there a charge for that?
When staff use a new medical term:
- Can you please write that word down for me – and how to say it?
- What does that word mean in ordinary language?
- Is there a picture or visual you could show me that would help explain what you are talking about?
- What is a good website to get more information about this?
When you are being shown new exercises or how to support, lift or position your child:
- Is it ok if I video those exercises on my phone so I can check back to them when we are doing them at home?
- That is very complicated – would it be ok if I recorded you on my phone explaining that so I can play it back to my whānau who weren’t able to come with me today?
- I want to check that I have understood the next steps from today’s visit – you are going to do this and this and this …… and I am going to do this ………… Is that right? Did I miss anything?
Questions to ask before a test or procedure:
- Why is the test being done? What will we know after the test that we don’t know now?
- What steps are involved? What do I need to do to get my child ready?
- How long will the test take?
- How long before we get the results? And how will we find out the results – will you ring, will our GP let us know or will we get an email or text?
- Are there any dangers or side effects?
- Are you able to explain the risks to me please?
- Will our child need to have an anaesthetic?
- Will they need to stay in hospital?
- Is there someone else whose child has had this procedure that I could talk to?
- Is there a video or something we could watch about the procedure?
- Will our child have to stay in hospital?
- Will I be able to stay with our child?